Road to recovery: Cancer in the COVID-19 era
Challenges accessing treatment and care
Even as Canada recovers from the pandemic, many patients already diagnosed with cancer continue to experience difficulty getting the treatment and care they require.
 Most notably, there is a significant backlog of surgeries and diagnostic procedures, due largely to the nearly 30% decrease in cancer surgery volumes in April and May 2020.1 While the number of surgeries performed returned to usual by the end of 2020, the system still has a long way to go before the backlog will be cleared, especially with many jurisdictions putting surgeries on hold again in January 2022 in response to the fifth wave of the pandemic.
Most notably, there is a significant backlog of surgeries and diagnostic procedures, due largely to the nearly 30% decrease in cancer surgery volumes in April and May 2020.1 While the number of surgeries performed returned to usual by the end of 2020, the system still has a long way to go before the backlog will be cleared, especially with many jurisdictions putting surgeries on hold again in January 2022 in response to the fifth wave of the pandemic.
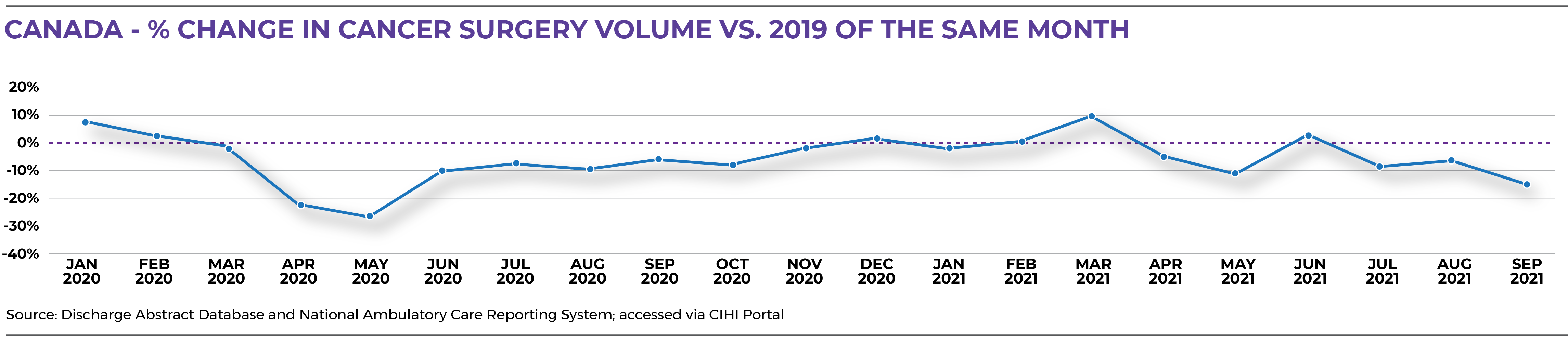
At the time of the production of the analysis provided here, the impacts of the disruptions caused by the delta and omicron variants of COVID-19 were yet to be fully quantified. Jurisdictions vary by the level of impact and timing of disruptions and delays — it will likely be months or even years before the system gets back up to speed. Until then, the pressure on the cancer system will intensify as diagnoses increase with the full resumption of screening services. That makes it critically important to maintain focus on cancer even as other types of surgeries ramp back up.
Other challenges related to treatment and care include:
A smaller bubble as a result of the pandemic has made it harder for us to gain a wider network of support, such as homecare.”
Cancer patient3
- In a 2021 survey by the Canadian Cancer Survivor Network, half of all cancer patients said their care appointments had been cancelled, postponed or rescheduled — a figure that climbed to 69% for patients with metastatic cancer. Patients waited an average of 28 days to reschedule care appointments and 44 days to reschedule surgeries, with 69% saying their emotional and mental health had been affected negatively. Even where clinics are operating at or near full capacity, getting people seen and treated sooner rather than later remains a challenge.4
- The need for social distancing during the pandemic has introduced more opportunities for virtual care, but inadequate internet access continues to be a challenge for many people including people living in remote and rural communities, people with low-income and people who have a first language other than English. And while virtual care can be a powerful tool when used appropriately, early evidence suggests it may not be as effective as in-person, hands-on assessments for diagnosing many kinds of cancers, so additional guidance on when and when not to use virtual care may be needed.5
I don’t mind the telephone appointments, but I wanted my oncologist to meet me in person so had to push for that. I think it’s important for the doctor to know who they’re dealing with.
Cancer patient3
- Discharge Abstract Database and National Ambulatory Care Reporting System; accessed via CIHI Portal
- Dare A, Anderson BO, Sullivan R, Pramesh CA, Andre I, Adewole IF, et al. Surgical services for cancer care. In: Gelband H, Jha P, Sankaranarayanan R, et al., editors. Cancer: Disease control priorities, third edition. Washington (DC): International Bank for Reconstruction and Development / World Bank; 2015.
- Canadian Cancer Society patient engagement survey. January 2022. Data available upon request.
- Canadian Cancer Survivor Network. Impact of COVID-19 crisis on cancer patients and their ability to receive treatment: 3rd survey. 2021. Available from: https://survivornet.ca/wp-content/uploads/2021/08/Survey-3-CCSN-Impact-on-Cancer-Patients-3rd-Report_July-30-2021.pdf
- Watson L, Qi S, Delure A, Link C, Photitai E, Chmielewski L, et al. Virtual cancer care during the COVID-19 pandemic in Alberta: Evidence from a mixed methods evaluation and key learnings. JCO Oncology Practice. 2021; 17(9):e1354-61.
