HPV vaccine access in Canada, 2022
Learn about the coverage of and eligibility for publicly funded HPV vaccines in each province and territory.
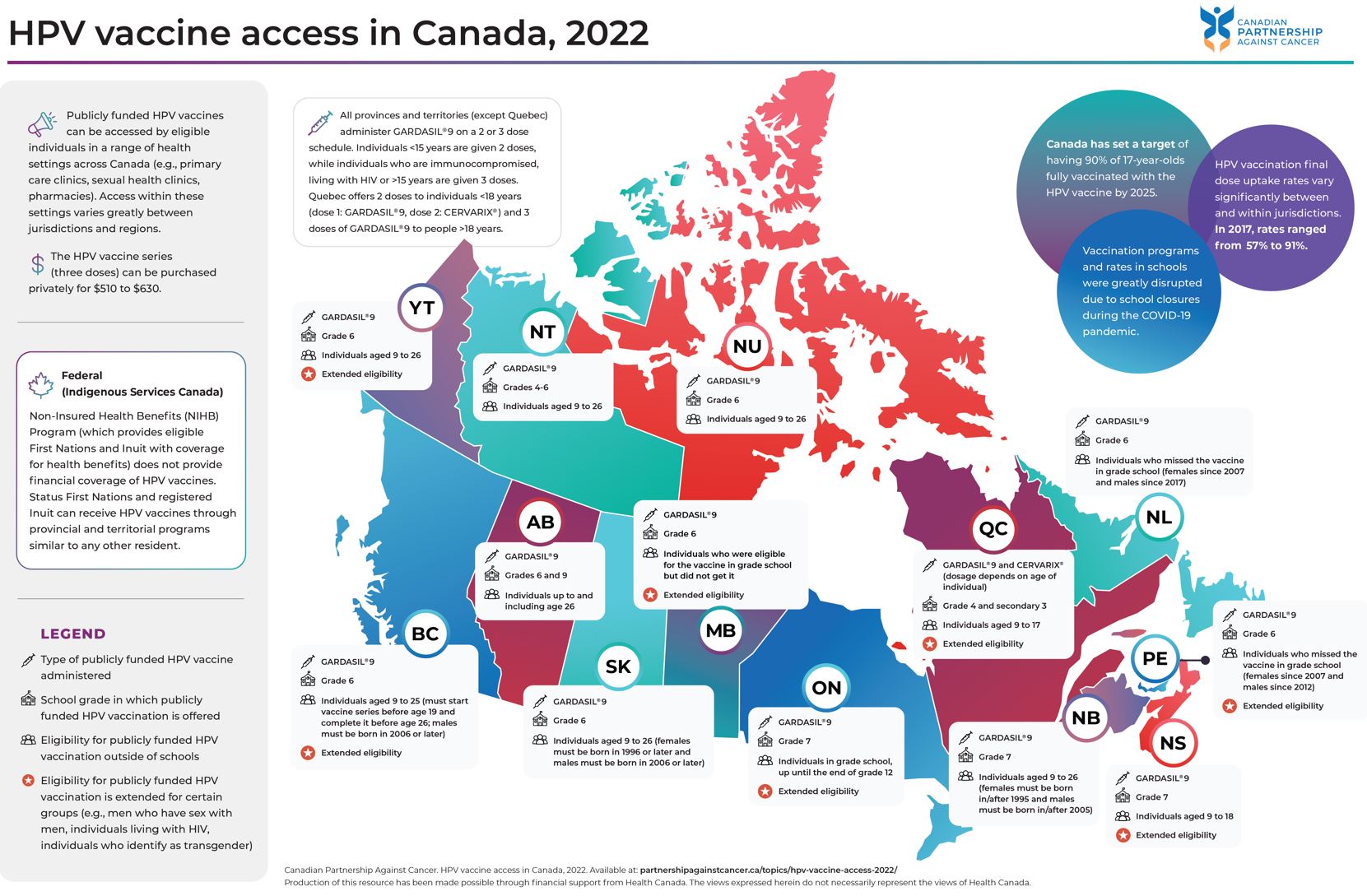
This resource provides information on who can get a free human papillomavirus (HPV) vaccine, where they can get it, and how much it costs to purchase it privately.
Download the map or click through the provinces/territories to learn more about differences in HPV vaccine access and coverage across Canada.
This map summarizes the publicly funded programs that provide financial coverage of the HPV vaccine. Eligibility for these programs varies significantly from jurisdiction to jurisdiction. Gaps in financial coverage and access to HPV vaccines create barriers in protecting the population against HPV infections and HPV-related cancers.
Click on the image to download a full size version of the map.
Quick facts
- Cervical cancer is almost exclusively caused by HPV, and HPV infection also causes other anogenital cancers and oropharyngeal cancers.1
- Although HPV infections are common, some types can cause cells to become abnormal and precancerous which can lead to serious cancers. HPV infections are highly preventable through HPV vaccination.2
- HPV vaccination is one of three components of the Action Plan for the Elimination of Cervical Cancer in Canada, 2020-2030, which aims to set Canada on the path to eliminate the disease by 2040. Canada has set a target of having 90% of 17-year-olds fully vaccinated with the HPV vaccine by 2025.
- Free HPV vaccines are offered through school-based programs and catch-up programs in all provinces and territories in Canada. Individuals who do not qualify for these programs can privately purchase the HPV vaccine series (three doses) for $510 to $630.
- All provinces and territories (except Quebec) administer GARDASIL®9 on a two or three dose schedule according to the NACI recommended immunization schedule for HPV vaccines. Individuals under age 15 are given two doses, while individuals who are immunocompromised, living with HIV or over the age of 15 are given three doses.
- HPV vaccination uptake rates vary significantly between and within jurisdictions. The provincial/territorial final dose HPV vaccination uptake rate ranges from 57% to 91%. Very little data has been collected on the rates of HPV vaccination for sub-populations within provinces/territories.
- School closures during the COVID-19 pandemic disrupted vaccination programs in schools, resulting in many children missing doses of the HPV vaccine.3
Coverage for First Nations, Inuit and Métis
- The Non-Insured Health Benefits program does not provide financial coverage of HPV vaccines. Status First Nations and registered Inuit can receive HPV vaccines through provincial and territorial programs similar to any other resident.
- First Nations, Inuit and Métis populations may experience specific barriers to accessing HPV vaccines. Increasing uptake among First Nations, Inuit and Métis may require community-specific approaches.4
- First Nations, Inuit and Métis organizations and governments have called for more Peoples-specific data to inform HPV vaccination programs.5
Alignment with the Canadian Strategy for Cancer Control, 2019-2029
The Canadian Strategy for Cancer Control calls for the elimination of cancers caused by HPV through universal access to HPV vaccination programs for girls and boys. The Strategy calls for these programs to be delivered in a way that is sensitive to cultural and social norms of populations in Canada, including First Nations, Inuit and Métis.
 This resource primarily supports Priority 1: Decrease the risk of people getting cancer, Action 2: Adopt proven practices known to reduce the risk of cancer of the Strategy. View progress and data related to this priority work.
This resource primarily supports Priority 1: Decrease the risk of people getting cancer, Action 2: Adopt proven practices known to reduce the risk of cancer of the Strategy. View progress and data related to this priority work.
Action Plan for the Elimination of Cervical Cancer in Canada
In response to the World Health Organization’s goal to eliminate cervical cancer worldwide this century, the Partnership has coordinated efforts with a broad group of partners across the country to create the Action Plan for the Elimination of Cervical Cancer in Canada, 2020-2030. The Action Plan includes three priorities: improve HPV vaccination rates, implement HPV primary screening, and improve follow-up of abnormal screening results. Peoples-specific priorities and actions to address the specific inequities that First Nations, Inuit and Métis may experience in cervical screening are also included in the Action Plan. The Partnership is currently supporting jurisdictions across Canada to advance these priorities and create more equitable cervical cancer prevention, screening, and care.
Related resources
- The Canadian Strategy for Cancer Control
- The Action Plan for the Elimination of Cervical Cancer in Canada, 2020-2030
- HPV immunization for the prevention of cervical cancer
- HPV primary screening and abnormal screen follow-up for cervical cancer
- Cervical cancer screening in Canada: environmental scan 2021/2022
- Eligibility and Out-of-Pocket Costs for HPV Vaccines Across Canada, a rapid review prepared by the North American Observatory of Health Systems and Policies
- de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. International journal of cancer. 2017 Aug 15;141(4):664-70.
- Centers for Disease Control and Prevention. An Estimated 92% of Cancers Caused by HPV Could be Prevented by Vaccine. CDC Online Newsroom. 2019 [cited 22 October 2020]. Available from: https://www.cdc.gov/media/releases/2019/p0822-cancer-prevented-vaccine.html
- Diamond LM, Clarfield LE, Forte M. Vaccinations against human papillomavirus missed because of COVID-19 may lead to a rise in preventable cervical cancer. CMAJ 2021; 193(37).
- Henderson RI, Shea-Budgell M, Healy C, Letendre A, Bill L, Healy B, Bednarczyk RA, Mrklas K, Barnabe C, Guichon J, Bedingfield N, MacDonald S, Colquhoun A, Glaze S, Nash T, Bell C, Kellner J, Richardson R, Dixon T, Starlight J, Runner G, Nelson G. First nations people’s perspectives on barriers and supports for enhancing HPV vaccination: Foundations for sustainable, community-driven strategies. Gynecol Oncol. 2018 Apr;149(1):93-100. doi: 10.1016/j.ygyno.2017.12.024. PMID: 29605057.
- Canadian Partnership Against Cancer. Action plan for the elimination of cervical cancer in Canada, 2020-2030. Available from: https://www.partnershipagainstcancer.ca/topics/elimination-cervical-cancer-action-plan/