Canada
Impact of a smoking cessation in cancer care initiative
Access to smoking cessation supports in cancer care settings
Most people in Canada now have access to smoking cessation supports in cancer care settings because of the focused work of partners in provinces and territories. The proportion of cancer care settings that offer people support to quit smoking has increased dramatically in the last few years, bringing the country closer to the ambitious goal set in 2017: to provide smoking cessation in all outpatient cancer care settings by 2022.
In 2022-23:
- 95% (108/114) of cancer care settings reported offering people support to quit smoking
- 49% (56/114) of cancer care settings reported offering culturally appropriate supports to First Nations, Inuit and Métis with cancer
Percentage of cancer care settings in Canada offering smoking cessation, 2012-17 to 2022-23
From 2012 to 2017, 26 cancer care settings offered smoking cessation supports. In 2017-2018, 56 settings offered smoking cessation supports. In 2018-2019, 66 settings offered smoking cessation supports, and of these, 18 out of 66 settings offered smoking cessation supports that were culturally appropriate. In 2019-2020, 73 settings offered smoking cessation supports, and of these, 30 out of 73 settings offered smoking cessation supports that were culturally appropriate. In 2020-2021, 87 settings offered smoking cessation supports, and of these, 44 out of 87 settings offered smoking cessation supports that were culturally appropriate. In 2021-2022, 87 settings offered smoking cessation supports, and of these, 45 out of 87 settings offered smoking cessation supports that were culturally appropriate. In 2022-2023, 95 settings offered smoking cessation supports, and of these, 49 out of 95 settings offered smoking cessation supports that were culturally appropriate.
Implementation of smoking cessation in cancer care
All cancer care settings in Canada that offer smoking cessation follow evidence-based guidelines and models,1-3 consisting of the following elements:
- When people come to a cancer centre or clinic, staff ask them if they use commercial tobacco, and advise them about the benefits of quitting to improve their cancer treatment and overall health.
- In some settings, staff automatically offer or refer people for smoking cessation support (‘opt-out’), and in others, they ask people if they would like support to quit smoking (‘opt-in’).
- Some cancer care settings offer people behavioural counselling and/or free smoking cessation medications at the point of care, which can take place either in person or virtually at or around the time of people’s cancer care appointments. Others refer people externally to a quitline, community smoking cessation program or pharmacist. Many cancer care settings and/or external programs offer follow-up support to help people stay smoke-free.
- Culturally appropriate supports for First Nations, Inuit and Métis with cancer are available in several cancer care settings and through Talk Tobacco (Indigenous quitline run by the Canadian Cancer Society and available in some provinces).
Provinces and territories use the Implementation Checklist from the smoking cessation in cancer care Action Framework to assess their smoking cessation supports on six quality dimensions, and identify steps toward full implementation. In 2022-23, the average implementation level for Canada was silver.
Smoking cessation in cancer care implementation levels in Canada,
2022-23
| Province/ Territory* |
Overall level | Behavioural counselling | Pharmaco-therapy | Person-centred | Culturally competent | Partnership | Indicator measurement and reporting |
|---|---|---|---|---|---|---|---|
| YT |
GOLD | Gold | Gold | Pre^ | Silver | Gold | Silver |
| NT | SILVER | Bronze | Gold | Pre | Gold | Pre | Pre |
| NU |
SILVER | Bronze | Gold | Bronze | Silver | Bronze | Pre |
| BC | GOLD | Gold | Gold | Gold | Silver | Gold | Gold |
| AB | SILVER | Silver | Silver | Silver | Bronze | Silver | Bronze |
| SK | SILVER | Silver | Gold | Bronze | Bronze | Silver | Pre |
| MB | GOLD | Silver | Gold | Gold | Bronze | Gold | Silver |
| ON | GOLD | Silver | Silver | Gold | Silver | Silver | Gold |
| NB~ | GOLD | Gold | Gold | Gold | Bronze | Gold | Gold |
| NS |
SILVER | Silver | Silver | Bronze | Pre | Silver | Pre |
| PE | GOLD | Gold | Gold | Silver | Bronze | Gold | Silver |
| NL | GOLD | Silver | Gold | Gold | Silver | Silver | Gold |
| Average level | SILVER | SILVER | GOLD | SILVER | BRONZE | SILVER | SILVER |
*Data are available for only 12 of the 13 jurisdictions.
^Pre = Pre-implementation
~Reflects cancer centres in Horizon Health Network regional health authority only.
See the Smoking Cessation Action Framework Implementation Checklist for the scoring rubric.
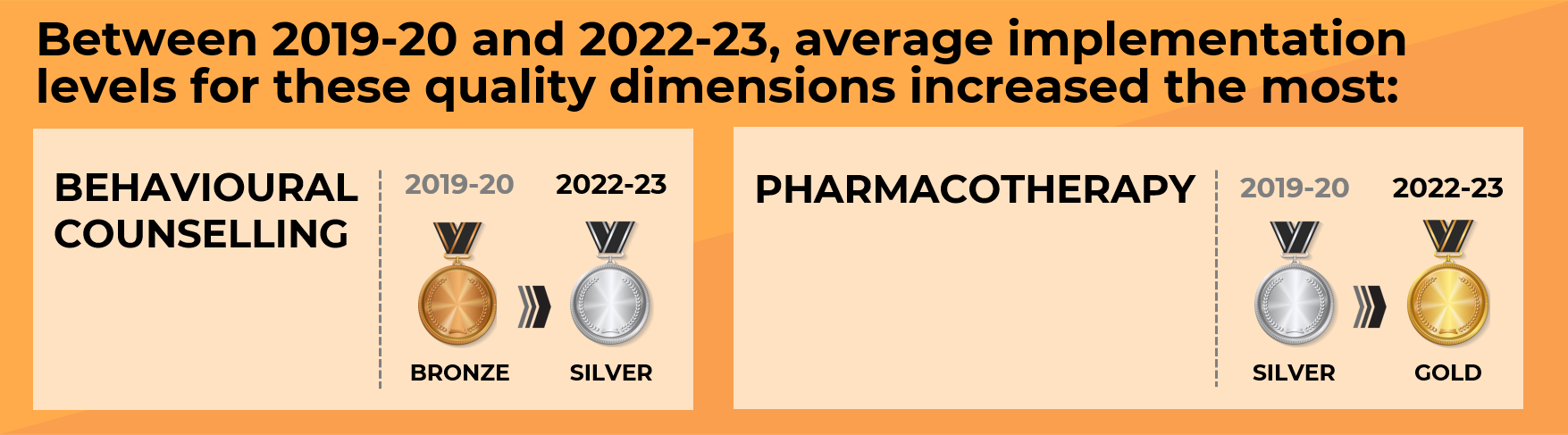
Provinces and territories have continuously strengthened their smoking cessation supports in cancer care settings. In the four years that these data have been collected (2019-20 data unpublished), the average score on the Implementation Checklist increased, despite the average medal (silver) remaining the same. Work is needed to continue to improve the implementation level of culturally competent smoking cessation for First Nations, Inuit and Métis with cancer, which is currently bronze.
Reach and effectiveness of smoking cessation supports
Smoking cessation supports reached many people with cancer; about a third of those who received support quit smoking. By the end of 2022-23, 10 provinces and territories were able to report on the reach of their smoking cessation supports during a median of 12 months. Although some jurisdictions were unable to report on certain indicators because of the way their referral systems were structured, seven jurisdictions’ programs were sufficiently established to be able to follow up with people and collect data on the effectiveness of the smoking cessation supports.
Reach and effectiveness of smoking cessation supports in cancer care settings at the end of funded projects, 2019-22
| Indicator | Median |
|---|---|
| % of people with cancer who were screened for commercial tobacco use | 76% |
| % of people who reported that they smoked commercial tobacco | 16% |
| % of people with cancer who reported smoking and were offered a referral for smoking cessation support* | 64% |
| % of people who accepted a referral for smoking cessation support* | 48% |
| % of people who received smoking cessation support and at follow-up said they had not smoked for the previous 7 days** | 32% |
*In some cancer care settings, people are automatically offered smoking cessation support at the point of care, rather than a referral.
**Five jurisdictions reported on the percentage of people at follow-up who said they had not smoked in the previous seven days. The timeframe in which this follow-up occurred was variable. Two additional jurisdictions only collected data at follow-up on how many people had not smoked for the previous six months, which was an average of 30% (not reported in table).
Economic evaluations
Manitoba and New Brunswick conducted economic analyses as part of their funded projects.
- CancerCare Manitoba found that its Quit Smoking Program (QSP) participants had lower healthcare costs compared to non-QSP participants who smoked, with the largest costs savings for people diagnosed with thoracic cancer.
- New Brunswick Cancer Network and Horizon Health Network collaborated with the University of Ottawa Heart Institute to conduct an economic evaluation of their smoking cessation program. When free smoking cessation medications were provided in the clinic, along with comprehensive follow-up supports, more people were ready to try to quit smoking. The increase in quit attempts significantly increased the number of people reporting they were smoke-free six months after the intervention compared to people who received smoking cessation support alone. Providing people with cancer smoking cessation supports and free smoking cessation medications was also highly cost-effective, with a high return on investment.
- A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. public health service report. Am J Prev Med 2008; 35(2): 158-76.
- U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. Smoking cessation. A report of the Surgeon General. Atlanta, GA; 2020.
- NCCN Clinical Practice Guidelines in Oncology. Smoking Cessation, Version 3.2022. Available at http://www.nccn.org.