HPV immunization policies
- Downloads
- Full report (pdf)
- Webinar slides (pptx)
Public perceptions of HPV immunization
![]() As the primary preventive tool against cervical cancer, ensuring that the public is adequately educated about HPV vaccination is critical. Lack of information about vaccine benefits is a barrier to HPV immunization uptake.
As the primary preventive tool against cervical cancer, ensuring that the public is adequately educated about HPV vaccination is critical. Lack of information about vaccine benefits is a barrier to HPV immunization uptake.
For example:
- More than half (52%) of parents of two-year-old children are concerned about the side effects of vaccines on their children, even though the majority (97%) agree that vaccines help protect the health of their children.
- Women who have not been vaccinated against HPV are more likely to express concerns about the safety of the vaccine (40% vs 26% of those who are vaccinated).
- The top barrier to vaccination is the lack of health care provider recommendations according to 38% of Canadians. Indicating physician partnership, as well as empowering people to inquire about HPV vaccination, will be key in the strategy to increase uptake of HPV vaccination.1
Health literacy and vaccine hesitancy
- Health literacy entails people’s knowledge and competence to access, understand, and apply health information to make decisions concerning their health.2
- Sixty percent of adults in Canada do not possess the level of health literacy required to manage their own health and healthcare needs.3
While health literacy of the public is highlighted as an important factor for healthy choices, it is not as straightforward concerning vaccine uptake.4,5,6
- The relationship between health literacy and immunization seems to be driven by risk perceptions and by the likelihood of becoming ill or suffering from complications in the short term.4 Thus, an individual’s high health literacy may only contribute to increased vaccine uptake if the health risks associated with HPV are accurately communicated to the public.
- Media, especially social media, tends to give mixed risk messages on vaccines’ efficacy, contrary to the evidence.4,7 According to the literature, social media from all sources tends to fixate on anecdotal stories of vaccine harms versus benefits.4,7,8 Regarding HPV, exposure to stories of harms resulted in less likelihood in proceeding with the vaccine.7
- This is especially important as social media is the dominant channel for driving conversation around cervical cancer and the HPV vaccine, which would have a definite impact on the public response.4,7,8,9 Studies have shown that providing information and educating parents about vaccination can change attitudes.10,11,12,13
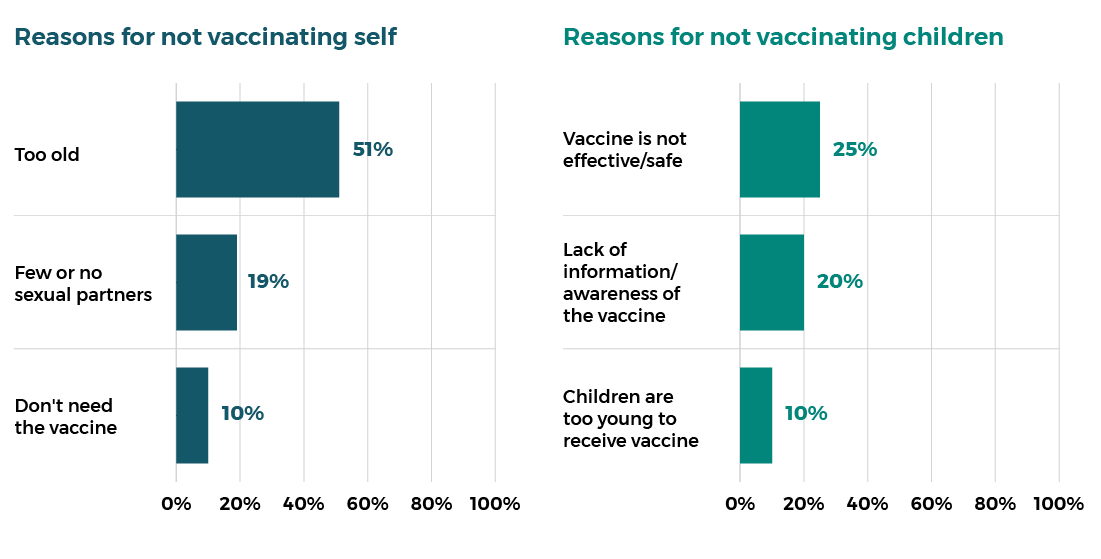
Decision factors to not receive HPV vaccination14
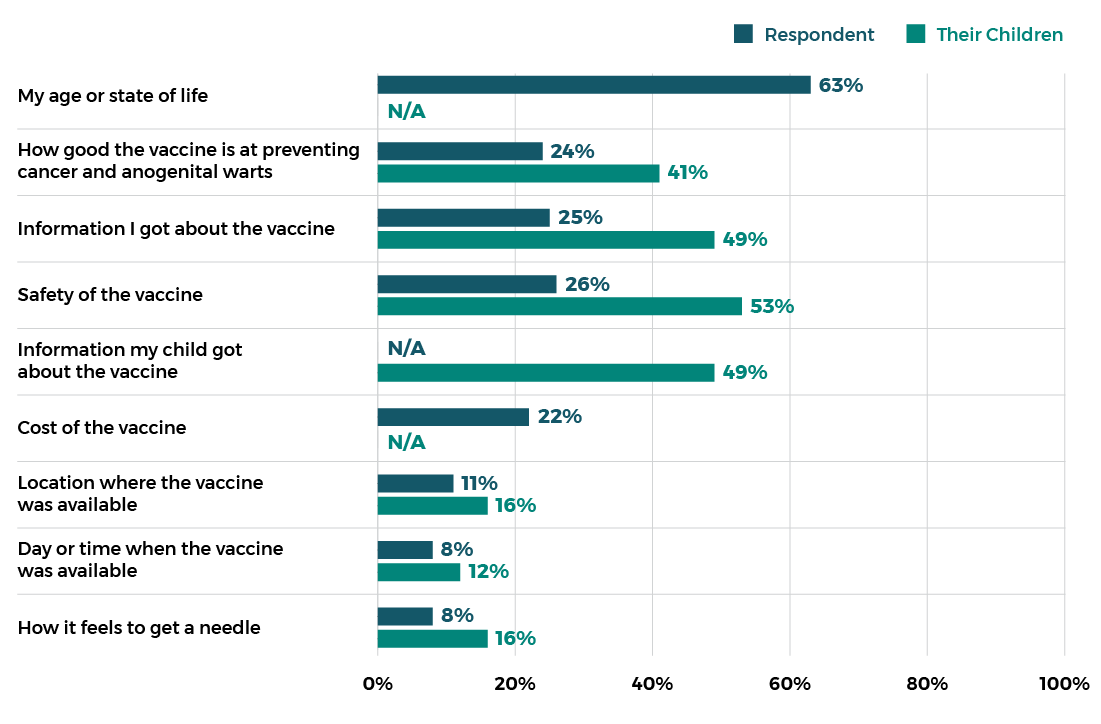
Reasons for not receiving HPV vaccination for self or children14
Religious or cultural objections
Although most religious and cultural groups agree with the use of vaccination, there nevertheless are some groups and individuals that oppose vaccination. Some of the common issues with vaccination that are raised include: ethical concerns associated with the use of human tissue cells or any animal tissue to create vaccines and beliefs that the body should be healed by a higher power, prayer, or other spiritual means.
-
References
1 - Gefenaite G, Smit M, Nijman H, Tami A, Drijfhout I, Pascal A et al. Comparatively low attendance during Human Papillomavirus catch-up vaccination among teenage girls in the Netherlands: Insights from a behavioral survey among parents. BMC Public Health. 2012;12(1).
2 - Pelikan J. From the Health Literacy Survey Europe (HLS-EU) to Measuring Population and Organizational Health Literacy (M-POHL). European Journal of Public Health. 2018;28(suppl_4).
3 - Hoffman-Goetz L, Donelle L, Ahmed R. Health Literacy in Canada; a Primer for Students. Journal of Cancer Education. 2014;32(2):211-212.
4 - Lorini C, Santomauro F, Donzellini M, Capecchi L, Bechini A, Boccalini S et al. Health literacy and vaccination: A systematic review. Human Vaccines & Immunotherapeutics. 2018;14(2):478-488.
5 - Amit Aharon A, Nehama H, Rishpon S, Baron-Epel O. Parents with high levels of communicative and critical health literacy are less likely to vaccinate their children. Patient Education and Counseling. 2017;100(4):768-775.
6 - Veldwijk J, van der Heide I, Rademakers J, Schuit A, de Wit G, Uiters E et al. Preferences for Vaccination. Medical Decision Making. 2015;35(8):948-958.
7 - Margolis M, Brewer N, Shah P, Calo W, Gilkey M. Stories about HPV vaccine in social media, traditional media, and conversations. Preventive Medicine. 2019;118:251-256.
8 - Meyer S, Lu S, Hoffman-Goetz L, Smale B, MacDougall H, Pearce A. A Content Analysis of Newspaper Coverage of the Seasonal Flu Vaccine in Ontario, Canada, October 2001 to March 2011. Journal of Health Communication. 2016;21(10):1088-1097.
9 - Edelman. (2019). Elimination of Cervical Cancer Landscape Analysis (Rep.). Toronto, ON.
10 - Wilson L, Rubens-Augustson T, Murphy M, Jardine C, Crowcroft N, Hui C et al. Barriers to immunization among newcomers: A systematic review. Vaccine. 2018;36(8):1055-1062.
11 - Smulian E, Mitchell K, Stokley S. Interventions to increase HPV vaccination coverage: A systematic review. Human Vaccines & Immunotherapeutics. 2016;12(6):1566-1588.
12 - Kang H, De Gagne J, Son Y, Chae S. Completeness of Human Papilloma Virus Vaccination: A Systematic Review. Journal of Pediatric Nursing. 2018;39:7-14.
13 - Niccolai L, Hansen C. Practice- and Community-Based Interventions to Increase Human Papillomavirus Vaccine Coverage. JAMA Pediatrics. 2015;169(7):686.
14 - Public and Patient Engagement to Inform Action Plan for Elimination of Cervical Cancer in Canada – Canadian Partnership Against Cancer, 2020. Unpublished Report.
- Downloads
- Full report (pdf)
- Webinar slides (pptx)
